Implementation of the open face mask and surface-guided radiation therapy system for the brain - PDF Version
With the installation of the Varian EDGE radiosurgery system in the University Clinical Center of Serbia, conditions for the application of stereotactic radiotherapy (SRT) and/or stereotactic radiosurgery (SRS) at the most advanced level have been met. An integral part of this system is the surface-guided radiation therapy (SGRT) optical surface monitoring system (OSMS). The target patients to be treated through use of this method are those with brain metastases of up to 4cm in diameter, for whom treatment can improve their quality of life, and patients with benign brain tumours of volume up to 10cm3. Other target groups comprise patients with metastases on bones, lungs, liver etc.
SRT/ SRS involves the application of large target doses in one to five fractions. Usually, this approach is used to treat brain matastases or benign brain tumours. The application of these techniques is demanding and requires sub-millimetre precision. In addition to the technological prowess of the system, the required precise execution of the treatment demands exact positioning and immobilisation of the patient as well as repositioning for repeat treatments. In order to meet these demands, we use Qfix Encompass Fiberplast SRS open face masks, the design of which is compatible with the SGRT OSMS system.
Between May 2019 and September 2021 we treated 600 patients with brain metastases or meningeoma through use of this type of face mask for positioning and immobilisation and we used the SGRT OSMS for the repositioning of patients on the linear accelerator (LINAC). The masks comprise two components: one part for the head and the other for the face. The set also includes a bite block and a hair cap that prevents hair from sticking to the mask during the procedure. We use the bite block for all patients with preserved dentition. The SGRT OSMS system is used according to the vendor’s instructions. The step-by-step procedure is as follows.
- Patient is identified in the OSMS system; patient selection and planning is easy in a system with basic data.
- Creation of DICOM computerised tomography (CT) field; this step involves creation of a field that contains information about the position of the radiation isocentre and the structure of the region from a CT simulator.
- Determination of region of interest (ROI); this is the most important step in the procedure. The outer line of the mask must be followed, including the eyebrows, nose, forehead, cheeks; we must try to ensure that there is a small gap between the edge of the mask and the ROI; the eyes must be covered to prevent interruption of the treatment due to blinking.
- Creation of an additional monitoring field; a field is created that will serve to obtain a position after verification in cone beam computed tomography (CBCT) (reference capture) and to monitor the patient during the radiation therapy.
- Repositioning and CBCT verification; the SGRT system enables highly precise repositioning with margins of less than 3mm for all axes.
- Implementation of therapy with monitoring by use of OSMS; the implementation is based on the field created for monitoring patients during the treatment.
The main result is the improvement of immobilisation and the achievement of the maximum possible precision of repositioning. We have found that the Qfix Encompass Fiberplast SRS open face mask is complicated for modelling but provides maximum security and at the same time is acceptable to the patient. The compatibility of the mask with the SGRT system provides for quick handling and the chance to adjust the position of the patient along the vertical axis with use of the integrated shim system on the mask. During the work, we have noticed and solved problems that the SGRT system has pointed out to us. These include:
- difficulty with a gap between the head and the mask – in a small number of cases, after the cap has been removed, a millimetre gap has remained during modelling of the mask, which causes the head to move. This problem was solved by following the SGRT directions over the longitudinal axis;
- patients without dentition cannot use the bite block and this leads to movement over the pitch axis – in this case, it is necessary to move the head in order to define the position according to the SGRT instructions;
- based on the OSMS, we have concluded that, during modelling of the mask and during the first positioning, the patient's head must be in a neutral position as far as is possible; large extension or flexion leads to an increase in the pitch axis;
- it is necessary to place the patient’s whole body as straight as possible in line with the sagittal laser, in order to avoid large rotation of the patient. To achieve this, it is desirable to use a knee-pad to enable the patient to take up a more comfortable and natural position;
- in most cases, we remove eye-tracking from the ROI, but on rare occasions, depending on the patient’s status, a rapid blink can interrupt radiation for a second and we must cover the eyes to determine the ROI;
- during mask modelling, the mask must be as close as possible to the face in order to avoid the creation of a small gap between the mask and the face.This gap can cause rotation or lateral movement of the head. This is solved with the use of integrated shims on the mask; and
- differences between the SGRT and CBCT can indicate malfunction in the SGRT system.
If the machine is used regularly for daily quality work, it is necessary to perform system quality assurance every three months. Deviations in the correct alignment of the SGRT system can be noticed even when there are large differences between the SGRT and the CBCT. The SGRT points out all repositioning errors and enables precise repositioning. The system has taught us to improve the patient’s position to the level that is required for this procedure. We followed the above-mentioned steps and observed problems that acted as an initial guide for this procedure. The data that we obtained have helped us to produce departmental guidelines for radiation therapists (RTTs), which we have included in national guidelines for RTTs.

Ilija Čurić
ead RTT
Radiosurgery and stereotactic radiotherapy department
University Clinical Center of Serbia
Serbia, Belgrade
iccurici@gmail.com
.jpg.aspx)
Patient on couch table
.jpg.aspx)
Determination of ROI Positions of treatment margins
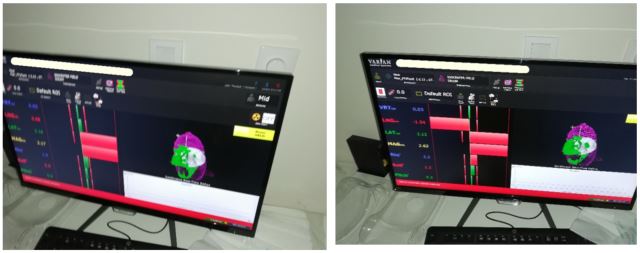
Repositioning according to SGRT directions Repositioning according to SGRT directions
.jpg.aspx)
Repositioning according to SGRT directions