Ultrafractionated radiotherapy(RT) in localised prostate cancer:HDR brachytherapy vs stereotactic RT
OC-0040
Abstract
Ultrafractionated radiotherapy(RT) in localised prostate cancer:HDR brachytherapy vs stereotactic RT
Authors: Yat Man Tsang1, Hannah Tharmalingam2, Katherine Belessiotis-Richards3, Shreya Armstrong1, Peter Ostler2, Robert Hughes2, Roberto Alonzi2, Peter Hoskin2
1Mount Vernon Cancer Centre, Radiotherapy, Northwood, United Kingdom; 2Mount Vernon Cancer Centre, Clinical Oncology, Northwood, United Kingdom; 3Mount Vernon Cancer Centreq, Clinical Oncology, Northwood, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To compare the biochemical progression-free survival (bPFS), late gastrointestinal (GI) and genitourinary (GU) toxicities in patients with low- and intermediate risk prostate cancer (PCa) treated with high-dose-rate brachytherapy (HDR BT) of 19Gy/1 fraction, 26Gy/2 fractions, or stereotactic ablative radiotherapy (SABR) of 36.25Gy/5 fractions.
Material and Methods
Between August 2008 and December 2017, patients with low- and intermediate risk PCa who received single dose or 2-fraction HDR BT, or 5-fraction SABR at a single institution were included. bPFS rates for the whole population and the individual treatment groups were calculated using the Phoenix definition. Post treatment GI and GU toxicities were evaluated according to the CTCAE v4.0 guidelines.
Results
195 patients with low- and intermediate risk PCa were included in this study with a median follow up of 60.5 months. bPFS at 5 years was 86% for all patients, and 69%, 95% and 91% for the 19Gy/1 fraction, 26Gy/2 fractions and 36.25Gy/5 fractions groups respectively (Fig 1). The cumulative 5-year incidence rates of ≥grade 2 GI events in the 19Gy/1fr, 26Gy/2fr and 36.25Gy/5fr groups were 0%, 2% and 5%, respectively. Incidence rates in those treated in the 5-fraction SABR arm were significantly higher(p<0.05) than those treated in both HDR BT arms where no statistically significant difference between the two HDR BT groups was seen(p=0.15). The cumulative 5-year incidence rates of ≥grade 2 GU events in the 19Gy/1fr, 26Gy/2fr and 36.25Gy/5fr groups were 30%, 5% and 7%, respectively. No statistically significant difference was found between the 26Gy/2fr and 36.25Gy/5fr(p=0.29) treatment arms but incidence rates in these groups were significantly lower than those seen after 19Gy/1fr(p<0.05)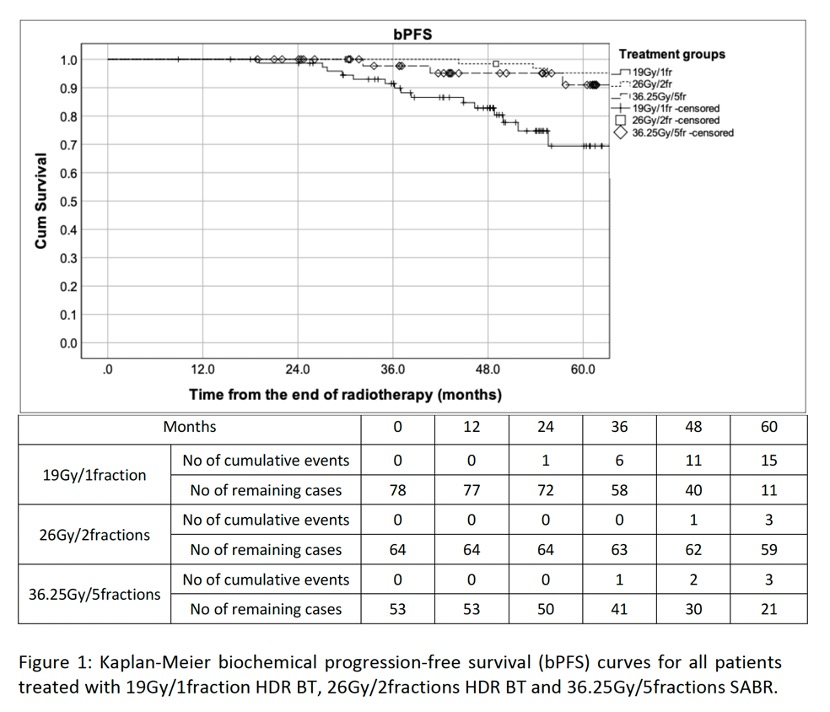
Conclusion
26Gy/2 fractions HDR BT provided equivalent bPFS with lower toxicity compared to 36.25Gy/5 fractions SABR. Both 2-fraction HBR BT and 5-fraction SABR achieved better bPFS than single dose 19Gy HDR BT. The two-fraction HDR BT schedule should be considered as an important comparator in future clinical trials.