Updated results of focal salvage high-dose-rate brachytherapy for radiorecurrent prostate cancer.
OC-0037
Abstract
Updated results of focal salvage high-dose-rate brachytherapy for radiorecurrent prostate cancer.
Authors: Max Peters1, Marieke van Son2, Marinus Moerland2, Jan Lagendijk2, Wietse Eppinga2, Taimur Shah3, Hashim Ahmed3, Jochem van der Voort van Zyp2
1University Medical Center Utrecht, Radiation Oncology, Utrecht, The Netherlands; 2UMC Utrecht, Department of Radiation Oncology, Utrecht, The Netherlands; 3Imperial College, Department of Urology, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Most patients with post-radiation prostate cancer recurrence undergo
palliative androgen deprivation therapy (ADT), since whole-gland salvage
treatments have a high risk of severe toxicity. Focal treatment of the
recurrence reduces this risk while offering a second chance at cure. The
objective of this study is to evaluate updated clinical outcomes of ultrafocal
salvage high-dose-rate brachytherapy (HDR-BT) and to explore potential risk
factors for treatment failure.
Material and Methods
We analyzed prospectively
collected data from the first 50 treated patients with locally recurrent
prostate cancer (treated between July 2013 and April 2017). Disease status was
assessed by 3T multiparametric MRI, 18F-Choline or 68Ga-PSMA PET/CT and
systematic or tumor-targeted biopsies. Ultrafocal salvage HDR-BT (1x19 Gy) was
performed by implanting the clinical target volume (CTV: gross tumor volume +
5mm margin) under fused TRUS/MRI guidance. Follow-up included toxicity grading
(using CTCAE 4.0), quality of life (QoL) assessment and PSA-testing. Potential risk
factors for biochemical failure (nadir PSA+2) were assessed.
Results
T-stage was T2
(62%), T3 (34%) and T4 (4%), Gleason ≥4+3=7 in 42%, PSA>10 ng/ml in 6% and PSADT<12 months in 16%. Median CTV D95% was 18.8
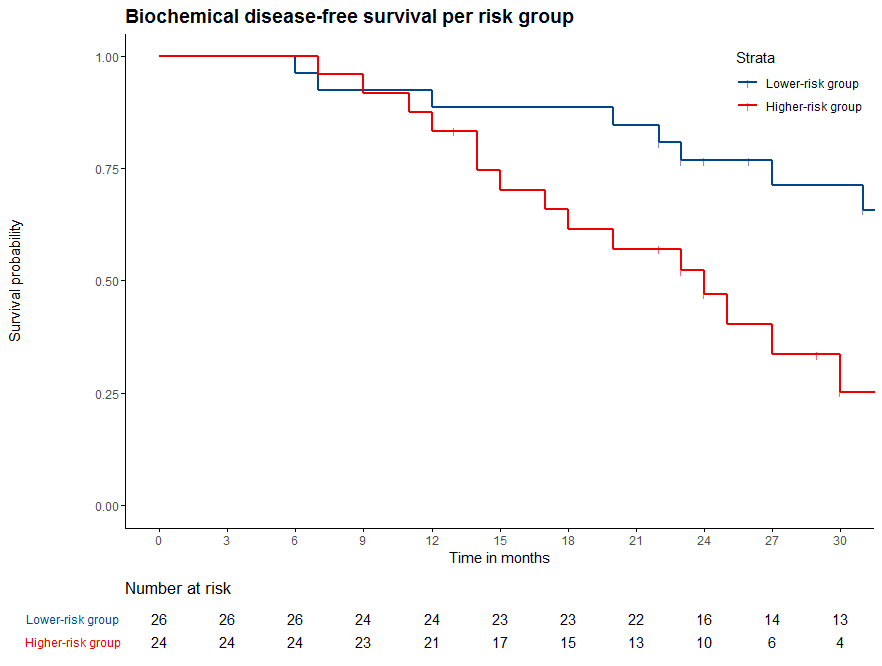
Gy. Median follow-up was 31 months. We observed
2% grade 3 genitourinary toxicity, no grade 3 gastro-intestinal toxicity and
22% grade 3 erectile dysfunction; 5/13 (38%)
with pre-treatment potency (IIEF>17) remained potent. Relevant but non-significant QoL deterioration was reported for social functioning,
mental health, tiredness, cognitive functioning and sexual functioning and
activity (6/31 items). Biochemical failure (BF)
occurred in 26 at median 20 months. Among intraprostatic
recurrences, 73% was in-field. After 2.5 years, biochemical disease-free
survival (BDFS) was 51% (95% CI 37-69%), metastases-free survival 75% (64-89%),
ADT-free survival 90% (82-99%) and overall survival 98% (94-100%) (Figure
1). "Higher-risk" disease (≥T3, PSA ≥10, or PSADT ≤9 months) had 25% BDFS at 2.5 years, against 71% for patients without (Figure 2).
Conclusion
MRI-guided ultrafocal
HDR-BT is a safe salvage treatment option, with a very low toxicity profile and
stable patient-reported QoL. It has acceptable biochemical control in a
well-selected group of patients and it can be an effective way to postpone ADT
(90% free after 2.5 years).
Figure 1:
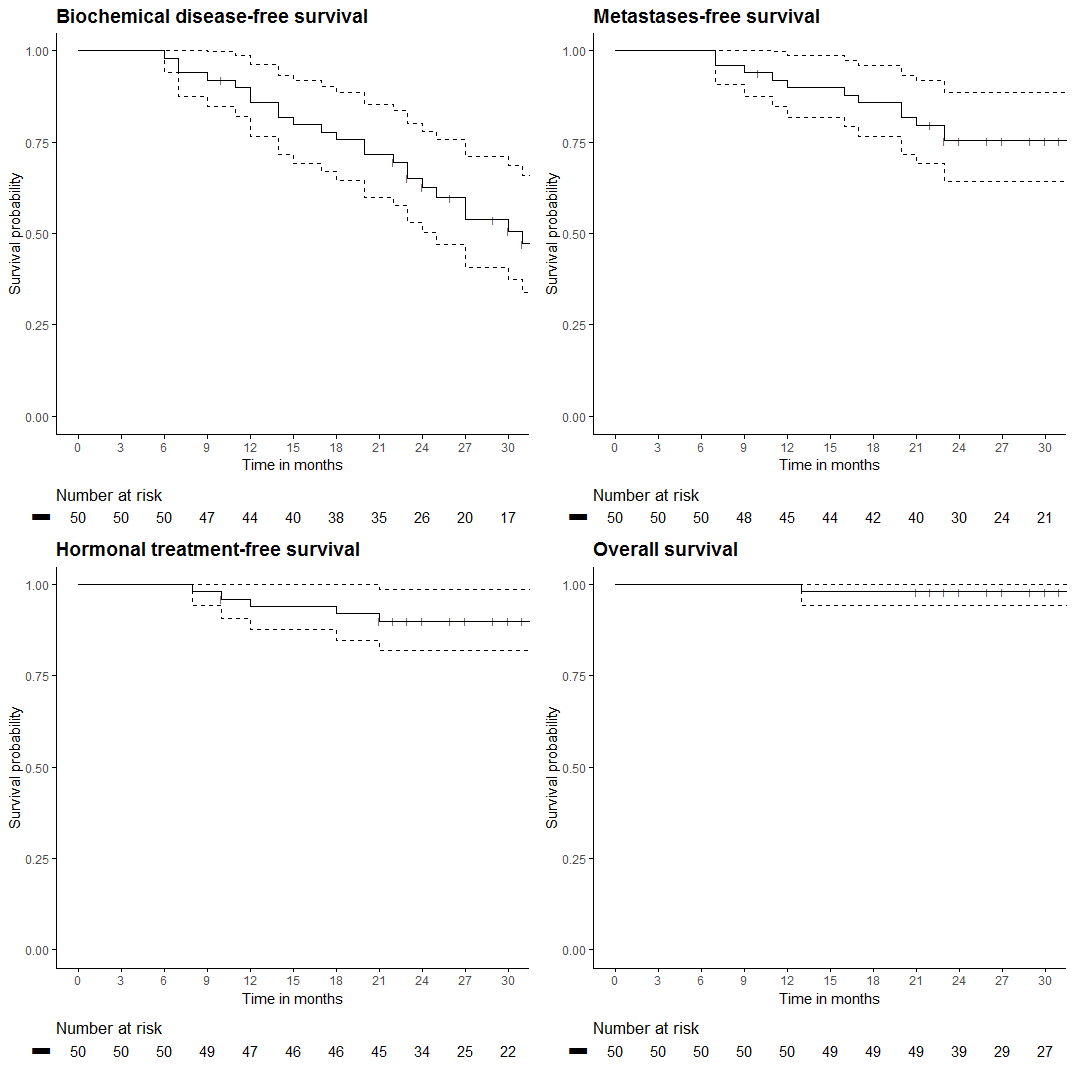
Figure 2: