Patients were stratified into four groups: (i) EBRT (n=12,985),
(ii) EBRT+ADT (n=12,960), (iii) BT (n=4,535), or (iv)
BT+ADT (n=1,303). Relative to EBRT alone, the following treatments were
associated with improved OS: EBRT+ADT (Hazard Ratio (HR): 0.92 [95% Confidence
Interval (95% CI): 0.87-0.97], P=.002), BT alone (HR: 0.90 [0.83-0.98], P=.01),
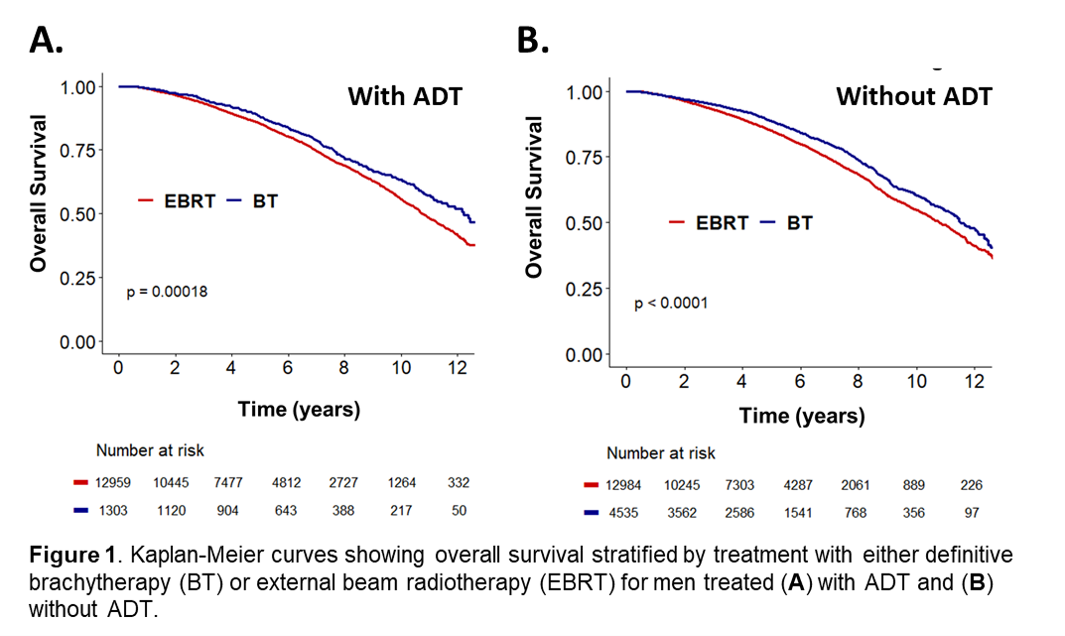
and BT+ADT (HR: 0.78 [0.69-0.88], P=.00006). In men receiving ADT,
brachytherapy correlated with improved OS relative to EBRT (HR: 0.84
[0.75-0.95]. P=.004) (Figure 1A). In men who were not treated with ADT,
brachytherapy correlated with improved OS relative to EBRT (HR: 0.92
[0.84-0.99]. P=.03) (Figure 1B). At 10 years follow-up, 56% and 63% of
men receiving EBRT and brachytherapy were alive, respectively (P<.0001).
IPTW was used to determine the average treatment effect of definitive brachytherapy.
Relative to EBRT, definitive brachytherapy was associated with improved OS (HR:
0.90 [0.84-0.97, P=.009) on weight-adjusted MVA. The addition of ADT was
associated with a similar improvement in OS (HR: 0.90 [0.83-0.97], P=.004).